BACKGROUND: Adult T-cell leukemia/lymphoma (ATLL) is an aggressive neoplasm of mature CD4(+) T-cells caused by infection by Human T-lymphotropic virus type1 (HTLV-1) ( Arch Pathol Lab Med PMID: 24476526). ATLL affects 5% of those infected by HTLV-1, mainly in Africa, the Caribbean, Japan, and South America ( Rev Assoc Med Bras (1992) PMID: 27925051). In the United States (US) it is usually seen in immigrants from these regions ( Arch Pathol Lab Med PMID: 24476526). While there are treatment options for ATLL, it is often refractory to conventional chemotherapy and in general has a poor prognosis ( Actas Dermosifiliogr (Engl Ed) PMID: 29685460, Cancer Treat Res PMID: 30596217). Considering its poor outcomes and unique epidemiology, more information is needed regarding its effect in Hispanics (HI) vs Non-hispanics (NH) in the US.
METHODS:
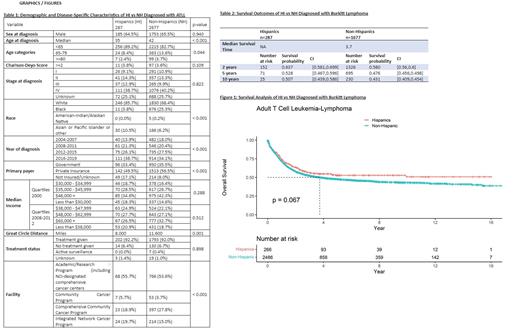
Data were analyzed on ATLL patients in the US reported to the National Cancer Database (NCDB) between 2004 and 2019. Demographic and treatment characteristics were compared between ethnic groups. Kaplan-Meier and Cox regression analyses were used to compare overall survival (OS) between HI and NH populations. Multivariate analysis and propensity score matching was performed with adjustment for age, stage, comorbidity score, and insurance status, type of facility and great circle distance.
RESULTS
Of the 3073 ATLL patients studied between 2004 and 2019, 9% were HI, and 87% NH. In both groups, most here male with 65% of HI and 66% of NH. At diagnosis, HI patients were younger with a median age of 35 years vs. 42 years in NH (p<0.001). HI patients were more likely to be <65 at diagnosis 89% vs 83% (p=0.044). Most HI and NH patients identified as white (86% vs 68%), followed by black (4% vs 25%).
Private insurance was the most common type in both groups (50% vs 57%), followed by government sponsored insurance (33% vs 36%). HI had a higher rate of being uninsured 12% vs 6% (p<0.001). Regarding Census Median Income (2008-2012), the most prevalent bracket for HI was $48,000 - $62,000 (28%), compared to NH $63,000+ (33%). HI were more likely to have an income of less than $38,000 (21% vs 18%) (p=0.512). HI also tended to live closer to their hospital (Great Circle Distance), with a median of 8.0 miles, vs NH at median of 11.6 miles (p=0.001).
On survival analysis; the survival probability at 2, 5 and 10 years of HI vs NH were (64% vs 58%), (53% vs 48%), and (51% vs 43%), respectively. The median survival (MS) time was 3.7 years for NH and not reached for HI. The overall survival (OS) difference favoring HI was marginal and non-statistically significant (p=0.067).
Independently, on multivariate analysis, NH ethnicity was not associated with worse OS (HR 1.25, CI 0.9-1.74, p=0.18). Interestingly, the propensity matched analysis demonstrated significant MS difference between HI vs NH (median 1.84 vs. 1.53 years).
CONCLUSION
Although the difference in OS in this study between HI and NH was not significant, there is a trend in the data showing increased survivability among HI despite patients in this group being more likely to be uninsured or in a lower income bracket. One possible explanation is that HI tended to present at an earlier age when compared to NH. It is evident that more data is needed to increase the power of these findings. Therefore, further study into the disease differences between these two groups, early detection, tumor markers, and targeted treatments will be necessary to improve the overall poor prognosis of this aggressive disease.
Disclosures
Diaz Duque:AstraZeneca: Consultancy; Genentech: Consultancy; Morphosys: Consultancy; Lilly: Consultancy; ADCT: Consultancy.